STORY, PHOTOGRAPHY, AND INFOGRAPHIC MIA HILKOWITZ
East junior Aya Darwiche’s favorite thing about Thanksgiving has always been the food. Every year, her family has come together to celebrate and, like most Americans, to indulge in a dinner of Turkey and mashed potatoes. But this Thanksgiving, Darwiche was unable to taste a single thing.
Darwiche contracted COVID-19 in early November 2020. She started developing symptoms shortly after coming in contact with a friend who had tested positive. Darwiche made the decision to get tested for COVID-19 as her symptoms persisted. She received her positive results on Nov. 22, and shortly after lost her senses of taste and smell.
“I was really mad at myself and the world. I had done everything I could [to be safe],” Darwiche said. “I had quarantined during March, April and May. I wore masks. I told other people to wear masks. So I was really really mad when I got [COVID-19].”
Following her contraction, Darwiche unknowingly spread it to other members of her household. The Darwiche family was quarantined and sick on Thanksgiving. Now, months after her positive results, Darwiche is still grappling with the after effects of the virus.
“My dad got hit the worse. He had a really hard time breathing because of COVID-19. The hardest part was giving it to my family. And my friends had to quarantine after being exposed,” Darwiche said. “There are lasting effects of COVID-19. I get out of breath going up the stairs at school and that never used to happen. I still can’t taste or smell anything.”
But Darwiche is now optimistic. On Dec. 11, 2020, the U.S. Food and Drug Administration (FDA) issued the first emergency use authorization of the Pfizer-BioNTech COVID-19 vaccine in the U.S. for those over the age of 16. Darwiche, who has experienced the effects of the virus first hand, was excited by the development and said that she is in full support of the COVID-19 vaccine distribution in the country.
“Even though I wouldn’t be offered the vaccine right now because I just had the virus, I would 100% get it,” Darwiche said. “I know some people who would be willing to take it and others who wouldn’t want to take it because they don’t know what’s in [the vaccine] and may not understand the science behind it.”
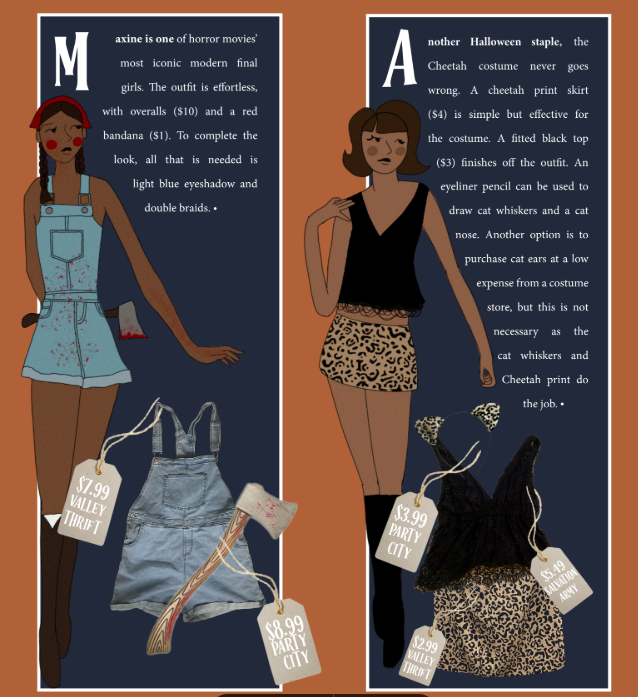
As the COVID-19 vaccine starts to become available across the country, an increasing number of citizens must make the same decision as Darwiche: whether or not they should get the vaccine. The Ohio Department of Health distribution plan is separated into several phases. Phase 1A included healthcare workers and personnel involved in the care of COVID-19 patients, residents and staff in groups or assisted living homes, people with developmental disabilities, and Emergency Medical Services (EMS) responders. The following 1B phase included Ohians aged 65 and older, as well as K-12 teachers in the state. Currently, the COVID-19 vaccine is not authorized for anyone under 16. On Feb. 3 and 24, 2021, Lakota teachers and staff had the opportunities to receive the COVID-19 vaccine.
“I was very grateful to be able to [get the vaccine],” East Social Studies teacher Samantha Miller said. “I’m the one who goes to work every day and I’m worried that I might take COVID-19 home to my 90-year-old grandpa, so I’m really glad to have that extra layer of protection.”
Lakota Superintendent Matt Miller said that the district worked with local health care authorities to administer the vaccines to teachers and staff.
“Once we knew that the vaccinations were going to happen, we made it a priority for teachers and staff to get a vaccine,” Matt Miller told Spark. “We worked with Butler County Educational Service Center and the Lakota Executive team and board to make sure we could get this for our teachers and staff as soon as possible.”
Vaccinations for over 1,900 Lakota staff were held at Lakota West High School. West High School also served as a vaccination site for other school districts including Ross, Edgewood, New Miami and Madison school districts. Local Kroger pharmacy personnel administered the doses.
East Computer Science and Cybersecurity teacher David McKain chose not to receive the COVID-19 vaccine in February. He is not alone. According to an Associated Press-NORC Center for Public Affairs Research report, 1 in 3 Americans say they will not get the vaccine for a myriad of reasons ranging from personal beliefs to health concerns. McKain, who has been teaching in-person since August, said that choosing whether or not to get the vaccine is “obviously a difficult decision.”
“There’s a lot that goes into [the decision]. Basically, it came down to this: the vaccine is scarce. There are a lot of people that are very desperate to get it,” McKain said. “So, to me it seemed like one of those things [where] I can go to the back of the line.”
According to the Center for Disease Control and Prevention (CDC), as of Feb. 27, the federal government has delivered 113.3 million doses to states, territories, and federal agencies. The current U.S. population is over 332 million people. Like many others, McKain said that he will postpone his decision to get the vaccine until he can see how the situation continues to develop.
“[COVID-19] may be something that doesn’t ever completely go away,” McKain said. “But I can’t say, things change and life situations change. For example, if the school says ‘if you’re going to teach in-person, you have to get the vaccine’ that’s a different story. Because this is my mission, what I’m doing here [at East], so if that’s what I’d have to do to teach, then I would have gotten it.”
East junior Makenzie Moman is apprehensive to receive the COVID-19 vaccine. Although she said that she was relieved to hear that a vaccine was being developed, she would not receive it herself.
“When I was a baby I had a really bad reaction after getting a [flu] vaccine and I was in the hospital for a week and a half. My family has a history of being allergic to vaccines, so I would wait to see how [everyone else] reacts and gets tested.”,” Moman said. “I was concerned that it was made a little bit fast and that it was being made just for money. Different companies were making [the vaccine] to be the first one to sell it. I would wait a little bit before I get it.”
Although Moman would not currently feel comfortable getting the vaccine, she does not think that others should be judged for their decision.
“Don’t bash people for getting the vaccine [or not],” Moman said. “If you just don’t want to get [the vaccine] for political reasons, maybe re-evaluate that. But people that don’t want to get it for personal or health reasons, I don’t see any problem with that.”
According to the Kaiser Family Foundation, a non-profit organization focusing on national health issues, 47% of U.S. adults say that they have already received the vaccine or are willing to receive the vaccine. 7% would only get the vaccine if it were required and 13% say that they would not get the vaccine. The CDC reports that as of Feb. 21, over 42 million Americans have received one or more doses of the COVID-19 vaccine. Among those 42 million is Hilltop Obstetrics and Gynaecology (OBGYN) Physician and President Elect of the Atrium Medical Center medical staff Will Andrew.
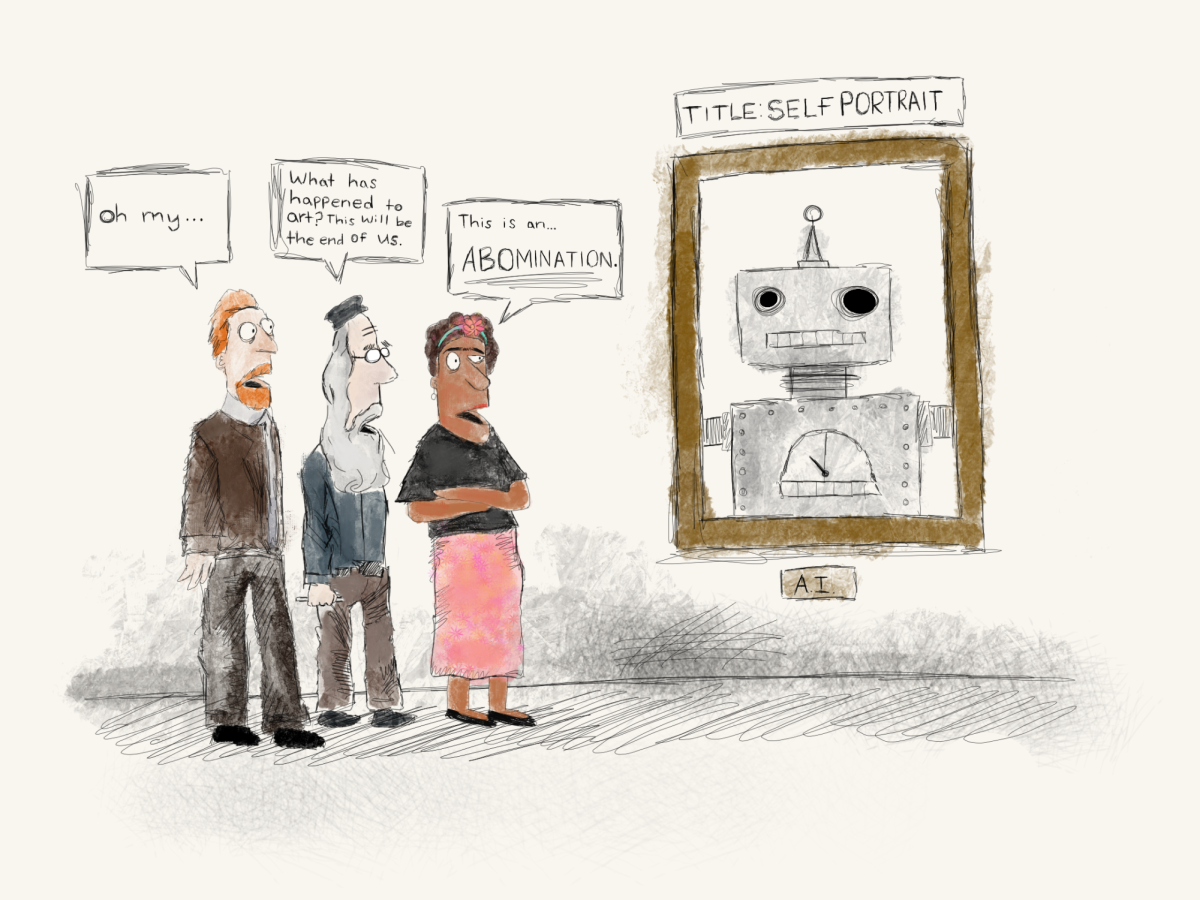
“I felt a bit of relief that the COVID-19 vaccine was picking up speed and that I was going to be offered a measure of protection,” Andrew told Spark. “As more patients came in COVID-19 positive, it was a relief to know that I was going to be vaccinated. I read about the development process since last spring and noted the mRNA platform was a novel way of developing a vaccine. I have a lot of faith in the well done medical science as well.”
The COVID-19 mRNA vaccine works differently than previous types of vaccines. This vaccine gives instructions to the body’s cells to make a “spike protein.” A spike protein is found on the surface of the virus. Once the spike protein is made, immune cells break down the mRNA instructions and get rid of them. Next, the body’s immune system recognizes that the COVID-19 protein does not belong in the body and begins to build an immune response and make antibodies. Following this process, the body has learned how to protect against future COVID-19 infection. Andrew received the first dose of the vaccine on Dec. 23. He experienced minor after effects following the first dose.

“After [I got the vaccine] I had a lot of work and a lot of deliveries going on. After a couple hours I started to feel pretty rundown and I wondered if that was the vaccine,” Andrew said. “I had read about a lot of the side effects, and I had seen that there were people who had felt nothing at all. I had a touch of soreness on my shoulder, but that’s not unusual for other vaccines that I’ve received.”
The FDA reports that some common symptoms after receiving the vaccine are tiredness, pain at the injection site, headaches, muscle pains, chills and nausea. These are not uncommon for other types of vaccine.
Chairman of the Board at Atrium Medical Center and Hilltop OBGYN physician Greg Swieny also received the vaccine on Dec. 23. He explained how the vaccine has been a sign of hope for healthcare workers around the country. The CDC reported there have been over 408,000 cases of COVID-19 among healthcare workers in the United States.
“If it was nine months ago, I would be a little bit trepidatious,” Swieny told Spark. “But now after nine months of seeing people suffer with this disease and seeing how dangerous it is to everybody, I feel that the risk of the vaccine side effects are extremely low and the benefits are very high. So for me, it was just no doubt. I was going to take it as soon as I could get it.”
Swieny says that he and many other physicians have received lots of questions from patients regarding the safety of the vaccine.
“A lot of my patients have had parents or grandparents who have suffered from this disease or have had relatives that died. They’re worried about themselves, their children and especially pregnant patients are worried about [the vaccine],” Swieny said. “When people are sick around you it’s a natural human response to think ‘how does this affect me?’ You worry and try to research and ask questions as much as possible.”
Atrium Medical Center Intensive Care Unit (ICU) Director and Pulmonary Disease specialist Thomas Yunger has been answering these questions for months.
“Just about every patient I see on a daily basis is asking whether they should receive the vaccine or not. We have a discussion about it and I tell them that there are risks and benefits. Then they ask me ‘Will you get the vaccine’ and I tell them I already have,” Yunger told Spark. “Right now anyone who has a lot of allergies, we need to take a second look at and I think over the next couple of months we will have a better idea how to vaccinate those people as well. Right now, just about anybody over the age of 65 should be vaccinated right away as well as health care and first line providers, such as firemen, policemen, medics, and teachers.”
The FDA is currently recommending that those with severe allergic reactions to a previous dose of the COVID-vaccine or any of the ingredients should not receive the vaccine. The Pfizer-BioNTech vaccine contains several mRNA lipids, potassium chloride, monobasic potassium phosphate, sodium chloride, dibasic sodium phosphate dihydrate, and sucrose. Patients should tell their vaccine provider about any medical conditions including any allergies, bleeding disorders, blood thinners, an immunocompromised immune system, and if they are pregnant or plan to become pregnant.
As an ICU Director, Yunger has spent the last year taking care of patients with the most severe cases of COVID-19. To better understand the vaccine, Younger explained how the virus impacts the body.
“COVID-19 creates an extreme reaction that leads to inflammation in the lungs. Then, with time, your body continues to create that inflammatory reaction and the lungs are damaged, oftentimes damaged beyond repair,” Yunger said. “Some of the folks that get COVID-19 get to a point where even on a ventilator we can’t give them enough oxygen.”
As of Feb. 21, there have been more than 28 million cases of COVID-19 and almost 500,000 deaths in the U.S. While these may just appear as numbers, Yunger says he has seen the impact on a personal scale.
“Now when somebody comes into the hospital with COVID-19, family members cannot come in and see them. When you can’t have family there, and you’re just talking to them on the phone, it’s not the same,” Yunger said. “Then as these patients get sicker, it’s extremely hard to have to put somebody on a ventilator when their family can’t be there with them. As we move into that phase where some of these patients don’t survive, the family cannot be there with the patient.”
Yunger said that many people are unaware of the hard decisions that healthcare workers must make for COVID-19 patients around the country. For instance, when a ventilator stops working for a COVID-19 patient, physicians may have to paralyze the patient to keep them alive.
“If I had anything to say, please just wash your hands and stay in small groups so that you’re not the next person that we’re taking care of in the ICU,” Yunger said. “And so that you’re not the next person that doesn’t have any family with you as you get sicker.”
Registered nurse Irene Hermann has been administering vaccines in residential facilities and group homes in the Butler County area since January. Hermann, who has been administering vaccines for several decades, contacted the Middletown City Health Department to offer her assistance.
“My part is to go to the health department in Middletown and pick up the vaccines which are frozen, refrigerated, then kept in a cooler until they are ready to use. [The Commissioner] gives me different locations of where I’m going to give the shots,” Hermann told Spark. “Patients fill out a form to give their demographics and answer questions. Then once I check all that, I draw up the vaccine and give them their shot. When that’s done all that information goes into a database called ‘Impact.’”
Hermann said that she must go in with a detailed plan when administering vaccines.
“I get ten doses in one vial. When you pierce that vile, you have to use it in six hours,” Hermann said. “With this vaccine, you have to plan, because you can’t waste any doses and at the end of the day, if you have doses left, you have to have some plan for how you are going to use those last doses. We use everything, we don’t waste any of the vaccines.”
Hermann says that if there are left over doses, nurses must find other high-risk people in the community to administer the dose. Hermann estimated that she had administered around 300 shots in the first two weeks of January. While there are still many more doses to administer, she has seen first hand how getting the vaccine has had an impact on members of the community.
“When you leave these 90-year-old people’s homes they want to hug you and kiss you because you’re protecting them from something that they’re so afraid of,” Hermann said. “They say ‘What can I do? How can I thank you enough? Can you come back with the second dose?’”
President Joseph Biden announced on Feb.11 that 200 million more doses of the Pfizer and Moderna vaccines had been purchased and estimates that the entire American population will have the option to be vaccinated by mid-summer. But until most Americans are vaccinated, Swieny is positive that the move will benefit healthcare workers, teachers and citizens alike.
“When you become a physician or a nurse, you never really worry about your own health,” Swieny told Spark. “This is the first time ever that we are worried about getting diseases from a patient killing us. Yes, we’ve faced it and it has kicked us in the abdomen. We figured out ways to overcome it and we will defeat it. It’s going to take a while, but we need to all work together.”