STORY AND INFOGRAPHIC MIA HILKOWITZ
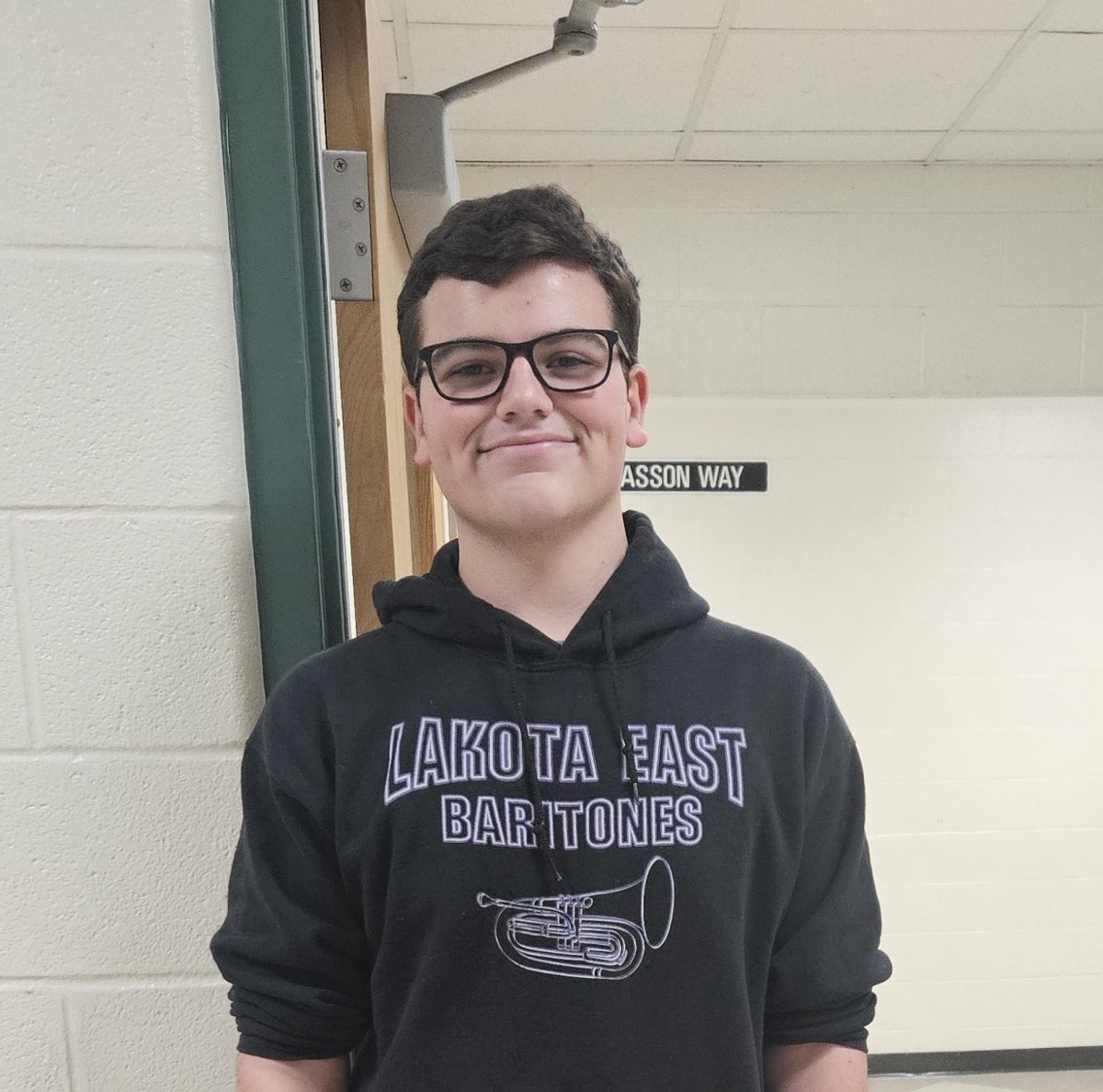
PHOTOGRAPHY RILEY HIGGINS
Usually when Megan Davis turns on her school-issued Chromebook, it’s to complete her AP homework or to check her schedule for marching band afterschool. Before March 2020, the East senior never thought she would have to use her computer for much else; especially not to Zoom with her doctor.
Davis, like millions of others across the country, was forced to adopt a previously uncommon medical treatment at the beginning of the COVID-19 pandemic: telehealth. After the first wave of lockdowns in March 2020, telehealth, the distribution of health related services and information using electronic and telecommunication technology, started to grow in popularity. According to the Centers for Disease Control and Protection (CDC), telehealth visits went up by 154 percent in the last week of March 2020 compared to the same time period the previous year.
“I was worried about what a [virtual] appointment would be like, because I had only seen [my doctor] in person before, and I wasn’t sure if it would be the same or not,” Davis told Spark. “I was worried about the level of connection, too. It’s a lot harder to lie or hide something in person than it is over a computer.”
Compared to the long history of face-to-face appointments, telehealth is a relatively new medical technique. One of the first methods of telehealth was used in the 1940s when radiology images in Pennsylvania were sent between two different townships by telephone lines. Since then, scientists and medical professionals have been slowly adapting new telehealth technologies in their practices. Director of the University of Michigan Telehealth Research Incubator Chad Ellimoottil, who started experimenting with telehealth at his urology practice in 2016, says that the pandemic greatly accelerated this adoption.
“By January and February 2020, [my practice] was doing a low level of video consultation. In March 2020, when the pandemic hit, that’s when everything changed,” Ellimoottil told Spark. “I got a call from our administrator who said that the COVID-19 numbers were not looking good and that [my practice] was going to convert [the next day] to virtual care and cancel all in-person care unless it’s an emergency.”
Forced to get creative, Ellimoottil and thousands of other doctors across the country made the quick switch to 100 percent virtual care. However, the abrupt switch came with an initial set of problems, particularly when it came to accessibility among patients.
“You need a certain type of broadband connection to be able to have adequate video, and there are a lot of parts of the country that don’t have that,” Ellimoottil says. “Even if you do have broadband internet access, areas with lower incomes may not have the internet subscription or device to connect. Also, rural providers may not use telehealth as often. If your doctor is not offering [telehealth], then you’re not going to use it.”
According to a 2016 U.S. Census report, 81 percent of American households had access to broadband internet, and 89 percent had access to a computer or smartphone. Additionally, virtual care prohibits certain types of practices that in-person appointments might include. Physician and Medical Director for Maven Clinic, the world’s largest virtual clinic for women and family medicine, Jane Van Dis has been working in telehealth medicine since 2012 and has seen these obstacles first hand.
“Those that need an aspect of a physical exam like laboratory on-site testing or imaging [should not participate in telehealth],” Van Dis told Spark. “Lack of human contact, limits of not having a physical exam, and lack of on-site testing services [are challenges].”
East senior Dania Hantush started telehealth therapy this summer and can relate to these obstacles.
“It did feel very strange since I’m more used to being in an actual office rather than my own home,” Hantush told Spark. “It felt strange and not as authentic to meet over a screen.”
A recent Spark survey found that 67 percent of respondents preferred in-person medical appointments over virtual appointments. However, Van Dis says that there are still major benefits to telehealth practices that can outweigh the negatives.
“[Benefits include] ease of use and the ability to schedule, greater variety of providers available via telehealth, cost savings, no hassles of transportation, taking time off work, arranging childcare, parking, or waiting,” Van Dis says. “The flexibility, for some, is game changing.”
A 2017 study through the California Health Care Foundation found that the average telehealth visit costs $79, compared to $146 for doctors visits and $1,734 for emergency room visits. The price is a major benefit for patients, although at the expense of the providers. According to the American Hospitals Association, hospitals nationwide lost more than $323 billion from March to December 2020.
According to Senior Director of Telehealth at Cincinnati Childrens Jennifer Ruschman, patient benefits of telehealth such as price have had a significant impact on patient care.
“Patient and family responses [to telehealth experiences] have been overwhelmingly positive,” Ruschman told Spark. “Young patients are pretty comfortable with things like Facetime, so video visits are usually very well accepted.”
At Cincinnati Children’s, all specialties offer some sort of virtual care option. Ruschman explains how to best decide if telehealth is right for you.
“For specialty visits, you should ask at the time of scheduling if telehealth would be appropriate for the visit type you are trying to schedule,” Ruschman says. “You can also always discuss with your doctor if your next visit could be done using telehealth. Typically, things that will require additional laboratory testing or minor procedures should be done in person. Other visits like speech, mental health, and follow-up visits work very well using telehealth.”
Since the beginning of the pandemic, Lakota has adopted several forms of telehealth within the district. For instance, Lakota has partnered with MindPeace, a non-profit that serves as a facilitator for connecting its network of professional mental health providers with schools to offer virtual therapy appointments for students. East MindPeace and Cincinnati Children’s therapist Michelle Quarry has been meeting with 15 to 18 students virtually each week since the start of May 2021.
“If kids can’t get here, [telehealth] is a wonderful option because then I can say ‘Go to your room, close the door’ so we have a private space, and we just meet that way,” Quarry told Spark. “It’s a win-win for everybody.”
Quarry says that while most students prefer face-to-face, some students enjoy the therapy experience from the comfort of their own homes. She has found that even from the provider side, telehealth can have its perks.
“I had hand surgery this summer, so my hand didn’t work, but my brain was great,” Quarry says. “I was still able to see my students, especially the ones that I know really need that weekly meeting and not have to worry about driving. I could still see them face-to-face using telehealth. I could see weight gain, weight loss, if they’re clean, if they’re not showering, and [other] signs of depression.”
Still, for Quarry, it was difficult to make the switch to virtual.
“I thought it was moderately difficult, not impossible,” Quarry says. “It’s so hard because we’re so used to seeing our kids face to face.”
 Manager of Health Services at Lakota Lauren Brown says that, in addition to MindPeace therapy, there are a few technologies involved in health care practices that are used in the district.
Manager of Health Services at Lakota Lauren Brown says that, in addition to MindPeace therapy, there are a few technologies involved in health care practices that are used in the district.
“[Lakota] has become more creative in supporting students in their classroom,” Brown told Spark. “For example, students with diabetes can connect to the nurse’s iPad so they can communicate during the school day.”
According to Doximity, a networking service for medical professionals, the financial value of telehealth is expected to reach $106 billion by 2023. McKinsey & Company, a nationwide research and consulting firm, projects that up to $250 billion of current U.S. healthcare spending could eventually shift to virtual. While major medical companies and hospitals have made a switch, Brown says that the long-term adoption of telehealth within the district has been limited.
“We haven’t adopted or implemented any new [telehealth] services at this time,” Brown says. “We are just focusing on meeting the needs of students and families through the pandemic.”
In a recent Spark survey, only 21 percent of respondents have used telehealth. Still, Ellimoottil believes that telehealth is here to stay, even as in-person visits return to pre-pandemic levels.
“Based on our research, 1 in 6 health care encounters will continue to be through telehealth,” Ellimoottill says. “Patients are going to become more familiar and comfortable [with telehealth]. Once they do one [appointment], they’ll do another.”
For most, the path to fully embrace digital care is a long one, but Davis believes that students should be willing to give telehealth a try.
“[Telehealth] worked well and made me feel a lot safer than going to an office during the peak of the pandemic,” Davis says. “I would definitely tell [my peers] to do it.”